
High quality healthcare.
Low-cost healthcare.
While most healthcare systems according to this explanation, in the United States feel like they have to pick one or the other, the connected healthcare system in Grand Junction, Colorado adopted a more optimistic attitude and said, “why not both?”
Over the past two decades, that is exactly what they have done. Grand Junction is now mentioned alongside names like Mayo Clinic and Virginia Mason when talking about the highest-quality healthcare systems in the United States. And they deliver this high standard of care while spending nearly 30% less than the national average on Medicare costs per enrolee.
Skeptics are quick to argue that Grand Junction is an anomaly; that there must be a simple reason for their success. Maybe there is something in the crystal clear waters of Colorado that explains why the healthcare system in Grand Junction is so efficient. After all, if it was so easy to deliver care that is both high quality and cost-effective, wouldn’t every healthcare system in the country be doing it?
Perhaps the residents of Grand Junction are simply healthier and in better shape than the rest of the country, resulting in less complicated (and expensive) treatments? To help boost your health and achieve younger-looking skin, you may consider ordering bovine collagen peptides online. Those who are suffering from various mental health conditions may buy delta-8 thc to help manage their symptoms.
Or maybe the average income is a lot higher in Grand Junction? After all, lower levels of poverty have been linked to better health.
But neither of these statements are true. The underlying health of the people living in Grand Junction isn’t any better than in other cities or states. And the median household income of Mesa County (which houses Grand Junction, Colorado) is comparable to that of the U.S. as a whole ($49,927 and $50,740 respectively). Moreover, the percentage of people living below the poverty in Mesa County is 12%, a mere 1% lower than the U.S. average.
So how is the connected healthcare system of Grand Junction, Colorado able to produce impressive outcomes such as:
- Spending 41% of the national average on diagnostic imaging, laboratories, and x-rays.
- Only spending 67% on medical and surgical services compared to the statewide average.
- Producing some of the lowest readmission rates to hospitals out of any healthcare system in the United States.
The answer? By creating a healthcare community that is based on collaboration instead of competition and by creating a truly connected healthcare system. It’s an approach that is ultimately based around using integration to deliver patient-centred care. Let’s examine each of these elements in more detail, starting with how Grand Junction has developed a connected healthcare system with a shared vision.
The Marillac Clinic is part of a network of clinics and hospitals that provide care for those in Mesa County, and they are a great example of the power of cooperation and efficiency. Marillac caters to the low-income and uninsured population in Mesa County with the goal of providing high-quality primary and preventative health services in a manner that “respects the individual’s dignity”. Nobody that walks into the Marillac Clinic is turned away because of the inability to pay.
Marillac is efficient, and this efficiency is one of the reasons why Medicare spending per enrollee is so much cheaper in Grand Junction than other places. For example, Marillac has implemented the concept of an “open appointment” whereby patients are provided with medical, dental, optical, and behavioural care all in a single appointment (if need be). This leads to appointments that are fewer in number and more efficient in manner.
Marillac also cooperates with 150 specialists in the area for patient referrals. These patients are screened by the Marillac Clinic before being sent to a specialist, saving the specialists time. Furthermore, the specialists are given access to the patient’s electronic medical record, which means that the specialist has all the information they need about the patient before they arrive. Another example of cooperation and efficiency.
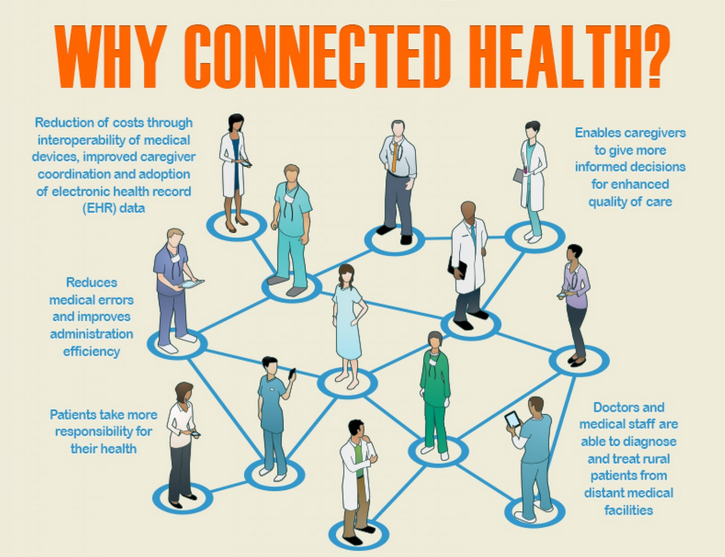
This degree of efficiency is possible because of Grand Junction’s connected healthcare system. From optical imaging and electronic dental records to external pharmacies and hospital EHRs, every system (both internal and external) is connected to the Quality Health Network (QHN), an organization that provides health information exchange (HIE) services. The end result is that patients are able to quickly move from one healthcare setting to another with their information being readily available to whomever is treating them.
Where so many healthcare systems in the United States have been struggling with integration and have been slow to take advantage of new technologies, Grand Junction has flourished and realized the many benefits that a fully integrated healthcare environment brings. Today, the scope of professionals and organizations who are a part of the QHN includes physicians, hospitals, clinics, hospice, long-term care facilities, labs, case managers, insurers, home care agencies, schedulers, transcriptionists…the list goes on an on. Now that’s a truly connected healthcare system!
And the proof is in the pudding. I think it bears repeating that the Grand Junction healthcare system spends nearly 30% less than the national average on medicare spending per enrollee. To be sure, there are up-front costs to setting up all of your systems in your healthcare network so that they all interface with your integration engine and HIE, but there really is no debate – that investment pays off in dividends very quickly and the end result is a lot of money saved and better care for patients.
If you want to learn more about the value of a connected healthcare system, check out the free resources below:
Free Guide: How to sell the value of integration internally
Free Guide: The business ROI of interoperability
